Uterine prolapse
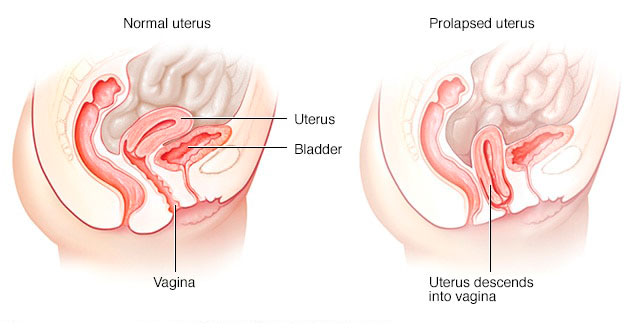
Uterine prolapse occurs when pelvic floor muscles and ligaments stretch and weaken and no longer provide enough support for the uterus. As a result, the uterus slips down into or protrudes out of the vagina.
Uterine prolapse can occur in women of any age. But it often affects postmenopausal women who’ve had one or more vaginal deliveries.
Mild uterine prolapse usually doesn’t require treatment. But if uterine prolapse makes you uncomfortable or disrupts your normal life, you might benefit from treatment.
Symptoms
Mild uterine prolapse generally doesn’t cause signs or symptoms. Signs and symptoms of moderate to severe uterine prolapse include:
- Sensation of heaviness or pulling in your pelvis
- Tissue protruding from your vagina
- Urinary problems, such as urine leakage (incontinence) or urine retention
- Trouble having a bowel movement
- Feeling as if you’re sitting on a small ball or as if something is falling out of your vagina
- Sexual concerns, such as a sensation of looseness in the tone of your vaginal tissue
Often, symptoms are less bothersome in the morning and worsen as the day goes on.
Causes
Uterine prolapse results from the weakening of pelvic muscles and supportive tissues. Causes of weakened pelvic muscles and tissues include:
- Pregnancy
- Difficult labor and delivery or trauma during childbirth
- Delivery of a large baby
- Being overweight or obese
- Lower estrogen level after menopause
- Chronic constipation or straining with bowel movements
- Chronic cough or bronchitis
- Repeated heavy lifting
Risk factors
Factors that can increase your risk of uterine prolapse include:
- One or more pregnancies and vaginal births
- Giving birth to a large baby
- Increasing age
- Obesity
- Prior pelvic surgery
- Chronic constipation or frequent straining during bowel movements
- Family history of weakness in connective tissue
- Being Hispanic or white
Complications
Uterine prolapse is often associated with prolapse of other pelvic organs. You might experience:
- Anterior prolapse (cystocele). Weakness of connective tissue separating the bladder and vagina may cause the bladder to bulge into the vagina. Anterior prolapse is also called prolapsed bladder.
- Posterior vaginal prolapse (rectocele). Weakness of connective tissue separating the rectum and vagina may cause the rectum to bulge into the vagina. You might have difficulty having bowel movements.
Severe uterine prolapse can displace part of the vaginal lining, causing it to protrude outside the body. Vaginal tissue that rubs against clothing can lead to vaginal sores (ulcers.) Rarely, the sores can become infected.
Prevention
To reduce your risk of uterine prolapse, try to:
- Perform Kegel exercises regularly. These exercises can strengthen your pelvic floor muscles — especially important after you have a baby.
- Treat and prevent constipation. Drink plenty of fluids and eat high-fiber foods, such as fruits, vegetables, beans and whole-grain cereals.
- Avoid heavy lifting and lift correctly. When lifting, use your legs instead of your waist or back.
- Control coughing. Get treatment for a chronic cough or bronchitis, and don’t smoke.
- Avoid weight gain. Talk with your doctor to determine your ideal weight and get advice on weight-loss strategies, if you need them.
Diagnosis
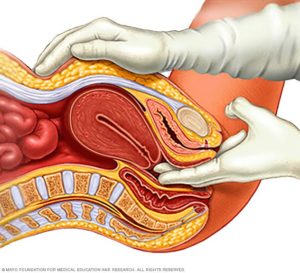
Pelvic exam
A diagnosis of uterine prolapse generally occurs during a pelvic exam.
During the pelvic exam your doctor is likely to ask you:
- To bear down as if having a bowel movement. Bearing down can help your doctor assess how far the uterus has slipped into the vagina.
- To tighten your pelvic muscles as if you’re stopping a stream of urine. This test checks the strength of your pelvic muscles.
You might fill out a questionnaire that helps your doctor assess how uterine prolapse affects your quality of life. This information helps guide treatment decisions.
If you have severe incontinence, your doctor might recommend tests to measure how well your bladder functions (urodynamic testing).
Treatment
Treatment depends on the severity of uterine prolapse. Your doctor might recommend:
- Self-care measures. If your uterine prolapse causes few or no symptoms, simple self-care measures may provide relief or help prevent worsening prolapse. Self-care measures include performing Kegel exercises to strengthen your pelvic muscles, losing weight and treating constipation.
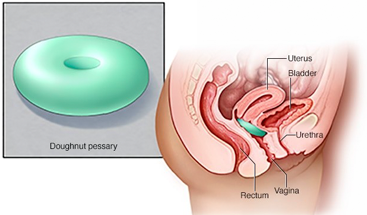
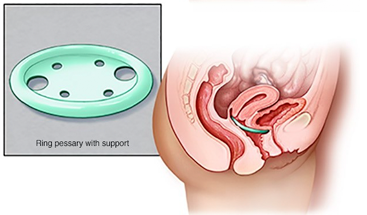
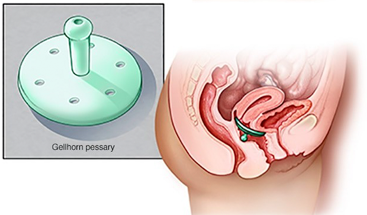
- Pessary. A vaginal pessary is a plastic or rubber ring inserted into your vagina to support the bulging tissues. A pessary must be removed regularly for cleaning.
Surgery
If uterine prolapse is severe, your doctor might recommend surgery. Minimally invasive (laparoscopic) or vaginal surgery might be an option. Surgery can involve:
- Repair of weakened pelvic floor tissues.This surgery is generally approached through the vagina but sometimes through the abdomen. The surgeon might graft your own tissue, donor tissue or a synthetic material onto weakened pelvic floor structures to support your pelvic organs.
- Removal of your uterus (hysterectomy). Hysterectomy might be recommended if uterine prolapse is severe. But hysterectomy is major surgery, and recent research suggests the surgery poses long-term health risks, including an increased risk of heart and blood vessel (cardiovascular) diseases and certain metabolic conditions.
Talk with your doctor about all your treatment options to be sure you understand the risks and benefits of each so that you can choose what’s best for you.
Lifestyle and home remedies
Depending on the severity of your uterine prolapse, self-care measures may provide relief. Try to:
- Perform Kegel exercises to strengthen pelvic muscles and support the weakened fascia
- Avoid constipation by eating high-fiber foods and drinking plenty of fluids
- Avoid bearing down to move your bowels
- Avoid heavy lifting
- Control coughing
- Lose weight if you’re overweight or obese
Kegel exercises
Kegel exercises strengthen your pelvic floor muscles. A strong pelvic floor provides better support for your pelvic organs, prevents prolapse from worsening and relieves symptoms associated with uterine prolapse.
To perform Kegel exercises:
- Tighten (contract) your pelvic floor muscles as though you were trying to prevent passing gas.
- Hold the contraction for five seconds, and then relax for five seconds. If this is too difficult, start by holding for two seconds and relaxing for three seconds.
- Work up to holding the contractions for 10 seconds at a time.
- Aim for at least three sets of 10 repetitions each day.
Kegel exercises may be most successful when they’re taught by a physical therapist and reinforced with biofeedback. Biofeedback involves using monitoring devices that help ensure you’re tightening the muscles properly for the best length of time.